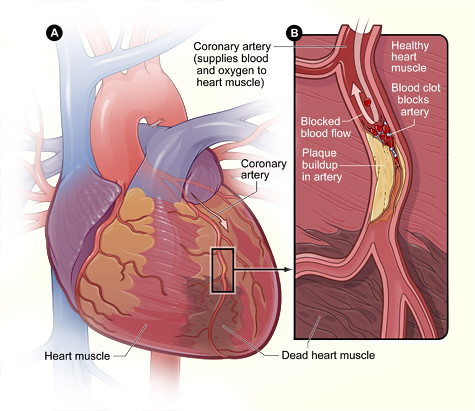
Coronary artery disease is the narrowing or blockage of the coronary (heart) arteries, as shown in the top illustration. After an interventional procedure, the coronary artery is opened, increasing blood flow to the heart.
Coronary artery disease is the narrowing or blockage of the coronary arteries caused by atherosclerosis. Atherosclerosis is the buildup of fatty deposits and inflammatory cells (called plaque) on the inner walls of the arteries that restricts blood flow to the heart. Without adequate blood flow, the heart becomes starved of oxygen and vital nutrients it needs to work properly. The most common symptom of coronary artery disease is angina, or chest pain.
When one or more of the coronary arteries suddenly becomes completely blocked, a heart attack (injury to the heart muscle) may occur. If the blockage occurs more slowly, the heart muscle may develop small collateral blood vessels (or detours) for other coronary arteries to reroute the blood flow, and angina occurs.
A complete blockage in a coronary artery is called a total coronary occlusion, or if it more than three months old, a chronic total occlusion.
Treatment for coronary artery disease involves a combination of lifestyle changes, medications and procedures to open up blocked arteries. Treating coronary artery disease is important to reduce your risk of a heart attack.
Common percutaneous interventional procedures to treat coronary artery disease includes balloon angioplasty (PTCA) and stent or drug-eluting stent placement. These procedures are considered non-surgical because they are done by a cardiologist through a tube or catheter inserted into a blood vessel, rather than by a surgeon through an incision in the chest.
A percutaneous coronary interventional (PCI) procedure may be the appropriate treatment option for patients who have poor blood flow through one or more coronary arteries.
Most patients with a symptomatic total coronary occlusion traditionally required coronary artery bypass graft (CABG) surgery to treat the blockage. Total blockages of the coronary artery have historically been the most challenging types of blockages to treat with an interventional procedure.
However, the emergence of new technology and new percutaneous techniques to treat total coronary occlusions allow experienced physicians to considerably improve the success rate of this treatment approach, making it a viable treatment option for patients who are experiencing symptoms related to these blockages.
Cardiac interventionalists are now using special guide wires and catheters that are gently steered across the total blockages. The fine movement of the guide wire tip is much easier to control than previous guide wire tips. In addition, at a very few centers in the United States, including the Cleveland Clinic, physicians use the "retrograde" approach, in which total coronary blockages are accessed from collateral blood vessels. Collateral blood vessels are new blood vessels that form to reroute blood flow around a blockage, and develop when the severity of a blockage increases.
Over the past few years, success rates with the combined percutaneous approach have increased from about 60% to 80-90%, if performed in experienced centers (in comparison to success rates of about 98% for percutaneous treatment of non-total blockages). The retrograde approach is not without potential complications, but the complication rate is only slightly higher than standard angioplasty, depending on the circumstances.
Each patient is evaluated to see what treatment options is best, based on the type of cardiovascular disease, the location of disease, patient’s age and co-existing medical conditions.